Intersex health and wellbeing: the role of parent counselling in two contrasting studies
A study published in the peer reviewed medical press this month describes the birth of an intersex child as a “challenging clinical emergency”, and finds that the incidence of post traumatic stress symptoms in parents is comparable to that amongst parents of children diagnosed with cancer.
OII Australia believes that the framing of the birth of an intersex infant as a “challenging clinical emergency” plays a very significant role in creating such stress, as does a lack of adequate counselling, peer support and contact with intersex adults.
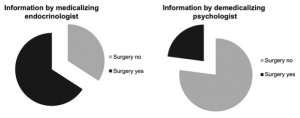
The implications of the pathologisation of intersex births for intersex children are known to be considerable. A second study shows that 66% of ‘parents’ who receive medicalised information choose early genital surgery for their child, while 23% do so if they receive demedicalised information.
Pasterski, Mastroyannopoulou, Wright, Zucker (that Zucker) and Hughes authored a paper entitled Predictors of Posttraumatic Stress in Parents of Children Diagnosed with a Disorder of Sex Development in Archives of Sexual Behavior, in February 2014.
The paper makes a number of statements – including the framing of an intersex birth as a “challenging clinical emergency”, with reference to a 2009 paper by Hewitt and Warne of the Royal Children’s Hospital, Melbourne:
[An intersex] diagnosis, defined as a condition where chromosomal, gonadal, or anatomical sex is atypical, presents a challenging clinical emergency: Immediate and long term concerns include gender assignment, genital surgeries, gonadal malignancy, potential gender dysphoria, and disclosure to parents and patients (Hewitt & Warne, 2009; Sutton et al., 2006)
The paper found a high incidence of post-traumatic stress symptoms (PTSS), astonishingly comparable to a cancer diagnosis:
Both mothers and fathers reported overall levels of PTSS that were comparable to those reported by parents of children diagnosed with other disorders, in this case cancer (Kazak et al., 2004).
It also documented sample size and other sample limitations typical of studies of intersex people:
In terms of limitations, we experienced relatively low participation, though this is consistent with similar studies including patients with a DSD (Crissman et al., 2011; Duguid et al., 2007; Slijper et al., 2000). This may in part reflect parents’ wish to avoid such a difficult subject matter. In two cases of non-participation, the reason given was that the parents wished to avoid any reminders of the child’s diagnosis. Such reasoning suggests that rates of PTSS in parents of children with DSD may well be higher than reported here. Avoidance behavior features prominently among PTSS. In addition, the largest cohort from which we invited participants, i.e., the CAH Support Group UK, had also been invited to participate in at least two other large scale studies being conducted in the UK at that time. In one study, many of the families were asked to return repeatedly over a 3 year period. It is very likely that many families were unable to make further efforts to participate in research.
The study also focused on infants and children with CAH, an intersex variation that requires immediate diagnosis and treatment to manage adrenal issues, which may potentially overstate parental stress. This CAH adrenal issue is not mentioned in the description of the “challenging clinical emergency”. It does not necessarily follow that a child’s genital configuration should be modified to fit social norms, but this is mentioned in the description of the “challenging clinical emergency”.
From OII Australia’s perspective, the framing of an obviously intersex birth as a clinical emergency and challenging disorder itself has direct and profound consequences in terms of the parents’ experience.
The nature of the clinical emergency as stated in the article includes issues around gender assignment, genital surgeries, sterilisation, and “gender dysphoria” (i.e. incorrect assignment). The primary focus is clearly on decisive actions to make the child fit social norms, rather than family counselling. Leaving aside clinician acknowledgement that cosmetic surgeries focus primarily on cosmetic outcomes, rather than sensation and sexual function, this illustrates a troubled nexus where an incorrect and potentially surgically-reinforced decision by clinicians and parents is treated as if it is a disorder in the patient.
Hughes, one of the authors, was a coauthor of the 2005/6 clinician “Consensus Statement” that replaced medical use of the word “intersex” with “Disorders of Sex Development” or ‘DSD” – a change that OII Australia opposes as it reinforces the idea that intersex traits are individual medical disorders that need to be fixed. The summary version of that clinician document identified rationales for genital surgery on infants that included “minimise family concern and distress” and “mitigate the risks of stigmatisation and gender-identity confusion”.
OII Australia believes that this medical model is not working in the interests of intersex children or families.
The paper Shaping Parents: Impact of Contrasting Professional Counseling on Parents’ Decision Making for Children with Disorders of Sex Development by Streuli, Vayena, Cavicchia-Balmer and Huber in the Journal of Sexual Medicine, August 2013, provides a marked contrast. It shows how the framing of initial counselling has a dramatically different effect on outcomes for infants (and, as a consequence, their families).
The management of disorders or differences of sex development (DSD) remains complex, especially with respect to parents’ decision for or against early genitoplasty. Most parents still tend to disfavor postponing surgery until the child is old enough to provide consent…
Parental decisions concerning early sex assignment surgery for DSD children depend on the health professional counseling received, to a degree of which neither parents nor professionals appear fully aware. In the absence of conclusive data for or against early surgery, there is a danger of medicalized or demedicalized parentalism resulting in irreversible and inadequately grounded decisions, regardless of the consensus statement of 2005 and the subsequent call for multidisciplinary management.
We want to see parents offered better peer support, including from intersex adults, not only demedicalised and non-pathologising counselling.
Parents subject to a situation framed as a “challenging clinical emergency” needing decisive action are going to make different decisions to those of parents offered demedicalised support and information. They are going to feel different about those decisions, and they’re going to feel different about their child. The consequences are irreversible and long lasting, for the whole family.
You must be logged in to post a comment.